By Madeline Strong Diehl
It all started from eating bad chicken, or so I thought. I lost everything in my stomach over a period of three hours, and the pain was only getting worse, so I called the answering service for my primary care doctor. It was early in the morning on May fifth, and a nurse instructed me to go to the U-M Hospital ER right away.
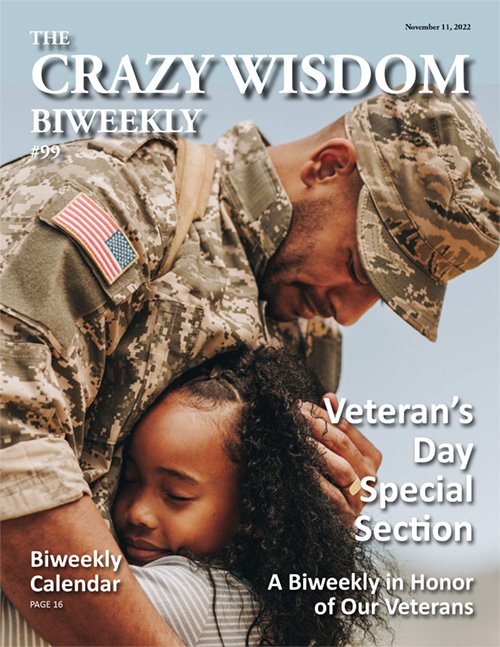
I had a lot of misgivings, mostly because I knew from a doctor friend that the U-M was still treating a significant number of people for Covid-19. Since April fourth the state of Michigan had the highest daily case rates and number of daily hospitalizations and deaths in the nation, and a large cluster of cases on the University of Michigan campus had contributed to that deadly surge. The ER was the last place I wanted to go. But when the pain in my abdomen became unbearable, my husband Ed insisted on taking me. He had to drop me off because of strict rules barring visitors.
I was screened twice for Covid upon entering the ER, so I knew the five other patients ahead of me had been thoroughly screened, too. All patients and staff were wearing masks. I’d had both doses of the Moderna vaccine, but its ninety-four percent efficacy rate still left me with a six percent chance of contracting Covid. While sitting in the waiting room, I tried to reassure myself that, if I did contract Covid, I would only get a “mild” case. But I had read about too many “mild” cases that were still pretty bad, because they could include pneumonia, loss of smell and taste, and being knocked off my feet with exhaustion for two weeks or more. After studying the data from Jan. 1-April 30th, the CDC had determined that 5-8% of all Covid cases were so-called “breakthrough cases” among people who were totally vaccinated. I felt foolish about opening myself up to these risks when I probably just had a bad case of food poisoning.
My fraught inner monologue was soon interrupted by a nurse who took my vitals and interviewed me about my symptoms. I didn’t have a fever, so I was surprised and alarmed when the nurse ushered me back to a triage area. When another nurse pricked me with a needle to establish a forearm IV and take blood samples, it was unnerving not to be able to see her face because of the mask she wore. Then I was taken back to an exam room.
I’ve never waited less than two hours to be seen by a doctor in the ER, but this time Dr. A., a resident of general surgery, entered after about twenty minutes. His dark beard was all but covered by his mask and he listened attentively as I explained that I had food poisoning from eating bad chicken. I ranked the pain in my abdomen as a seven or eight out of ten. He then put gentle pressure on the right side of my abdomen, below the ribs. I suppressed a scream, and I was soon given an ultrasound. After an hour or so, Dr. A., reappeared and announced, “It’s your gallbladder. We want to take it out while we have you here. We found sludge.”
I imagined a toxic waste dump located somewhere in my abdomen and felt even more exhausted and nauseous than I already was. What I thought was food poisoning was actually a gallbladder attack. Normally the gallbladder is helpful for the digestive process by storing and moderating the flow of bile, a substance that helps break down fat before it goes into the small intestine. But sludge, a build-up of small chemical particles, blocks the flow of bile and causes swelling and inflammation—a condition known as acute cholecystitis. CT scan images later showed that a calcified gallstone was also blocking the flow of bile between my liver and my gallbladder, causing an abscess. Dr. A. told me if I didn’t have my gallbladder removed, there was a chance it could rupture—potentially a life-threatening emergency. So, the other option, a two-hour laparoscopic surgery that afternoon, was a no-brainer. The surgery was over within about twelve hours of my arrival at the ER and I was released two nights later. I was told that I could go back to my normal activities in about a week, and the loss of my gallbladder would probably not affect me at all. Surgery to remove the gallbladder, a cholecystetctomy, is one of the most common surgeries in the United States, so it was no big deal. There was only about a three percent chance of complications.
Well, dear Reader, it turns out that, while almost all cholecystetctomies are textbook perfect, that still leaves a few of us who end up on the wrong side of statistics. Little did I know, my ordeal had just begun.
Before I go into the next chapter of this story, I have to warn you, dear Reader, that it is for mature audiences only because I am going to have to use a gross word, and that is pus. There is an equivalent medical term that sounds much more polite—purulence—but, to my mind, that word just cannot convey the feelings of horror and revulsion that I felt when I discovered a yellow-brown discharge coming out of my wound during an otherwise lovely spring day. It was the evening of Thursday, May thirteenth, and Michigan still had the highest Covid daily case rate and rates of daily hospitalizations and deaths. I had been out of the hospital just six days, but I felt strong and energetic, and I walked almost an entire mile with a friend. It was hot out, and I could feel moisture soaking through my T-shirt, which I assumed was sweat. But when I arrived back home, I discovered that a lot of pus was coming out of the largest of five incisions in my abdomen, where my gallbladder had been removed. So, my husband dropped me off at the ER for the second time in eight days. This time I was in the waiting room for more than an hour, and it had a completely different atmosphere from my first time. I overheard several patients being rude and aggressive toward staff about the policy barring visitors. In fact, one patient became so agitated that she began to threaten staff, at which point I believe she was taken to the Psychiatric ER—to the great relief of everyone else.
It occurred to me that screening for Covid and enforcing the no-visitors policy must be taking up a significant amount of time and energy of the already stressed-out and overworked medical staff. I guessed that this could only lead to some of them taking short cuts to save time, which might even cause mistakes. And during this visit to the ER, I personally experienced two things that, unfortunately, seemed to indicate that my hunch was correct.
Once I was ushered into an examination room, I recognized Dr. A. when he entered—the resident who had conveyed my diagnosis of acute cholecystitis during my first visit. Because all the medical staff was wearing masks, it was difficult to tell many of them apart, but Dr. A. was the only man I had encountered with dark hair and a full beard. He started treating my infection by putting me on a broad-spectrum antibiotic through an IV. Then he announced, “We’re going to have to open that wound back up and clean it out. This might hurt a little.” Then he asked another resident to hand him a scalpel from a rolling white instrument case. I instinctively put my hand up over my wound to protect myself and asked if he was going to give me any pain medicine. He said the whole process shouldn’t last long, so I didn’t need any. Then he began cutting all along the length of the incision, which was about two inches long. I begged for pain medicine, but he kept saying, “I’m almost finished. You’re doing a great job. I’m almost done….”
While he was cutting, I fantasized about channeling the spirit of my crazy Italian grandmother. I pictured myself grabbing the scalpel out of Dr. A’s hand, jumping off the bed, and brandishing my weapon. “Now, Dr. A., let’s find out more about your pain threshold!” But I knew that would certainly land me in jail. Still, just thinking about it helped reduce my pain level from a 9 to a 7.
My open wound was about an inch deep, and Dr. A. managed to squeeze out fifty milliliters of pus (or about two ounces. Don’t say I didn’t warn you that this is gross.) And only then, did a nurse administer fentanyl, a strong pain reliever and sedative.
By the time the fentanyl started working, it was too late; the damage had been done. To this day, I don’t know which was worst—the straightforward physical pain of being sliced into, or the emotional and psychological pain—the great vulnerability and helplessness I had felt. No doubt it was the combination of both that caused a psychological wound that was as big or bigger than my physical wound.
Dr. A. seemed to be oblivious to my emotional state and he asked me if I wanted to see the pus. I was so flabbergasted by the question that I couldn’t think of a reply. He then announced that he would teach me how to pack my wound. “How am I supposed to do that if I can’t see it?” I asked. (It was located below my right breast.) He suggested I could use a mirror, but there were about five steps involved and I couldn’t imagine keeping everything clean while also holding a mirror. I asked if my husband could please come in and learn how to do it. Even though guests were technically not allowed, the one exception was for teaching someone how to take care of a patient after release. So, Dr. A. relented, and another resident instructed my husband Ed on wound care. I was released from the ER shortly after midnight on Friday, and I couldn’t get out of there fast enough.
Prescriptions for two different antibiotics were called into my pharmacy, and I was alarmed when one of them turned out to be a sulfa drug, which appears all over my records as something I am allergic to. I had, and have, great respect for, and trust in, the U-M Hospital, so I could only assume that I was glimpsing some chinks in the armor of a world-class facility that had perhaps become strained by the demands posed by more than a year of dealing with the pandemic. In this context, it was only logical—and perhaps even predictable—that these otherwise brilliant, talented, and committed staff might make a few mistakes during the course of a particularly challenging shift. I had to assume that Dr. A. had not intended to cause me so much pain; he had probably been under a lot of stress and was probably also treating people with conditions much more serious than mine at the same time. Cutting into me and squeezing out the pus in my wound without giving me pain medicine first was probably a short-cut he felt he had to take under severe time restraints. I knew this intellectually, but emotionally, I felt an enormous amount of anger toward him—how could I not? I was deeply conflicted, because I knew anger was a highly toxic emotion that could interfere with my healing. I tried grounding myself in the present. I tried to use my mindfulness skills and prayed for Dr. A. every time an image of him arose in my mind and caused anger. I said the Buddhist lovingkindness prayer over and over in an effort to turn my negative energy around and lift up Dr. A. so that he would feel rested, capable, and strong; so that his mind and his heart could be up to the task of caring for so many people.
I wish, dear Reader, that my tale ended there, because that would be a nice place to end this. And I also wish that I did not have to keep mentioning the word pus. However, within one day of being released from the ER that time, pus began pouring out of my wound again. It was Sunday, May sixteenth, and at first I spent a couple of hours in total denial. Denial is a skillful way of putting off something unpleasant, but it also can have very bad consequences. Deep down I knew the longer I put off going to the hospital, the more I was allowing the bad bacteria in my body to multiply exponentially. Still, I just couldn’t bring myself to accept the reality that my infection was so darned stubborn. I had been resting and taking my antibiotics properly, but I was getting weaker and weaker as time passed.
My husband finally insisted on taking me back to the ER, and I scanned my bookshelves for a book that I could take with me to help me get back some sense of agency again. Instead, the book that called out to me was Pema Chodron’s When Things Fall Apart: Heart Advice for Difficult Times. The title pretty much summed up my life at that moment—I no longer felt that I was sitting in the driver’s seat of my life. I was a passenger in a car that was moving at a death-defying speed and careening from one collision to the next. I had read the book before, but I knew I needed to read it again, because it contained the essential Buddhist message that we are never actually in the driver’s seat of our lives. In fact, there is no car and there is no driver’s seat, and unless and until we accept that, we will cause ourselves great pain and suffering.
My husband is usually a very calm man, but I noticed that he was looking worried and strained when he dropped me off at the ER for the third time in eleven days. The ER was very crowded, but I was fast-tracked to an exam room, given an ultrasound and MRI, and again put on a broad-spectrum antibiotic through an IV. My infection had begun to kick my butt, and I was finding it difficult to find the energy and balance to get up and out of my hospital bed and walk to the bathroom. I was told I would be admitted, and I was interviewed by a surgery resident. “Do you know why this keeps happening to me?” I asked her.
“Sometimes with gallbladder surgery a nearby organ can get nicked,” she said.
“Nicked?” I asked, my anxiety level increasing by a magnitude of ten. She reassured me that they would do more imaging and if anything had gotten “nicked,” they could repair it. Not too long after that my nurse announced that they were in the process of assigning a bed for me in the acute surgery critical care ward. “Are you the patient who has MRSA?” she asked.
I was exhausted. I had not had any food for hours because they were still observing me and giving me tests. I had tried to stay polite with the staff, but at that point I lost my composure. “For God’s sake what is with you people?” I exclaimed. “First you tell me I might be nicked, then you mention I might have MRSA. Why can’t you just look in my records and find out the answer! There’s no need to terrify me anymore than I already am. I am more afraid of MRSA than Covid!”
“I didn’t mean to upset you,” the nurse said quietly, and while I couldn’t see her whole face—or the faces of anyone there, patient or staff—I became aware of the compassion in her eyes, which had been there all along. She asked if I would like more ice water or another warm blanket, and only then did I notice the white Styrofoam cup of ice water that I had been taking sips from. I appreciated how comforting it was to have a warm blanket covering my legs and torso. It reminded me of how my older sister tucked me in when I was a child. All this time, when the nurse had entered my room to take my vitals, she had also been making every effort to provide me with all the comfort she could offer. And I didn’t remember having ever thanked her.
“I’m so sorry,” I said. “You have been very kind and you have been taking very good care of me. Thank you so much.”
“Most patients are so distracted by their pain that they never thank us. So that means a lot to me,” she said. “Your room will be ready in half an hour, and then you will be able to get some good rest.”
Anyone who has ever spent the night in a hospital knows that it is very hard to get “good rest.” By the time I was settled into a room that night, it was midnight on May seventeenth, and my roommate was talking to her nurse about whether she was ready to die. They talked about her diagnosis—sepsis precipitated by a blood infection—and I overheard my roommate mention that she had been treated for sepsis at the U-M Hospital three times in the last four months. I tried not to listen to their discussion, but I was so tired and anxious, that I felt my roommate’s words almost physically.
I only got a few fitful hours of sleep that first night. I am terrified of MRSA and Covid, yes, but I am even more terrified of sepsis, and it was difficult to stop thinking about it when I knew that the woman on the other side of the room had been fighting it for four months. I like to think of myself as a kind person, an empath, but I was so exhausted and sleep-deprived that my anxiety revved into overdrive. I couldn’t seem to separate her situation from my own. Whenever I felt empathy toward my roommate, I felt anxious for her, too. Then I instantaneously became anxious for myself and imagined the worst possible outcome of my situation.
Dear Reader, have you ever had the experience of picking up a favorite book and opening it up at random to the exact page that you needed to read? At the point when I was giving up on ever falling asleep, I opened up my copy of When Things Fall Apart and found Pema Chodron’s description of tonglen—the Buddhist practice of “taking in pain and sending out pleasure” as a way to turn around our “well-established habit of doing the opposite.” She goes on to say, “Whenever we encounter suffering in any form, the tonglen instruction is to breathe it in with the wish that everyone could be free of pain. Whenever we encounter happiness in any form, the instruction is to send it out, with the wish that everyone could feel joy. It’s a practice that allows people to feel less burdened and less cramped.”
I became aware of how much emotional energy I was using to run away from my roommate’s pain and my own. Instead, I tried to become aware of the pain and let go of it on a moment-by-moment basis. I finally remembered that the way to get through difficult times is to stay anchored in the moment, with mindfulness—not look ahead toward some painless future which might always elude us.
I had definitely become traumatized by going to the ER three times in eleven days. Each of the two times I had gone before, someone had cut into me without a lot of notice, and I knew someone was probably going to cut into me a third time during this visit. I fell into a state of hypervigilance that made it impossible to sleep. I found myself in a place between dreaming and wakefulness, and I would startle awake whenever someone entered my room to check on me. It was dark, I was afraid, and I couldn’t see their faces behind their masks. In my mind’s eye each and every one of them became Dr. A. during the first few moments they were in my room. His words echoed over and over in my mind: This might hurt a little…hurt a little…hurt a little…. My sympathetic nervous system would kick in, my muscles tensed, and my mind ordered my body to flee. Each of these anxiety attacks lasted about half an hour to an hour, and then it would take me another hour to fall asleep—only to be awakened again by another nurse coming through the door.
Finally, morning came. Bright sunlight flooded the room, and nurses told me that my window looked out on the best view that the Acute Surgery ward could afford. Hardly any buildings interrupted the seemingly endless procession of trees that stretched out to the horizon. My mood also greatly improved when my nurse told me that I could eat real food for breakfast. I was just getting over my lingering feelings of dread and danger from the night before when suddenly Dr. A. entered my room, with the parade of medical students, residents, and the attending doctor that is known as “Grand Rounds.” Dr. A. immediately stepped toward me and asked kindly, “How are you feeling, Mrs. Diehl?”
I tried to keep my voice calm and steady in front of the other medical staff. “I am so glad I have the opportunity to see you again, Dr. A.” I exclaimed, and his eyes seemed to brighten above his mask, until I added, “I need to tell you that I was in terrible pain Friday night because you didn’t give me any pain medicine, and don’t you ever do that to another patient again!”
And in front of his colleagues, Dr. A. said, “Well, it shouldn’t have hurt that much because the nerves in the wound were dead from your surgery.”
This of course made me livid. “Are you saying you knew more about my pain than I did?”
One by one Dr. A’s colleagues discretely left the room. “I apologize,” he said. “That was wrong of me not to give you something for your pain. Thank you for telling me. This is a teaching hospital, and I am here to learn.”
I could tell he really did feel bad, and I reassured him that I forgave him. But the problem with forgiveness is that at first, it’s almost impossible to forgive someone one hundred percent. Forgiveness is a process, and even if we don’t really feel it at first, we must do our best to clear the way for it to happen. One must begin with the intention to forgive someone, and then go from there. We need to be true to ourselves if we still feel anger, and we also need to make a commitment to ourselves not to hold on to our anger. Anger is like an infection that can poison our blood. If we don’t let go of it, it can spread all through us, body and soul. I didn’t know how to bring resolution to the situation with Dr. A., and I ended up awkwardly holding out my hand. “Friends?” He shook my hand, and it was only afterward that I realized I hadn’t shaken anyone’s hand like that in more than a year. I figured that must be a sign of good intention.
I then met my roommate, and I was keenly aware that her condition was way worse than mine. She apologized for talking about her infection in my hearing the night before, and I told her I would pray for her, and asked her to pray for me. She told me she felt lucky to get a room, even a semi-private one, on a ward where there were no Covid patients. She said that during an earlier hospitalization that spring, she had stayed on a floor where non-Covid patients were mixed in with Covid patients. “I know there were Covid patients there because moonsuits were hanging outside some of the rooms,” she said. (NOTE: According to the U-M Hospital, the Covid Ward was closed in June 2020 and Covid patients were then treated on regular units including ICUs “with all appropriate infection control measures.”)
Dr. A. returned to tell me that images had revealed that the real site of my infection was not my incision, but below it, along the curve of my abdomen. I would undergo a procedure the next day to clear it out and wash the site, and they would take a culture to determine what kind of bacteria they were dealing with. I was so exhausted all I wanted to do was sleep, but nurses and physical therapists roused me regularly to walk to sustain my physical strength.
That night started out badly, and I was even more anxious than before. But I remembered to use my mindfulness skills and try to stay in the moment. I became aware of medical staff coming in and going out of my room every half an hour or so, making sure I was okay physically and emotionally, and bringing me ice water and warm blankets. I relished the fresh water—it had never tasted so good. When an alarm went off on one of my monitors around midnight, a male nurse entered who appeared to be seven feet tall. He assured me that there was no medical emergency; the monitor’s battery was just being finicky. Then he spoke gently with the monitor and tapped it a few times, telling it everything was okay and asking it to calm down. He then turned his attention to me. “Would you like me to tuck you in?”
I accepted without hesitation. “Excuse me for asking you a personal question, but are you seven feet tall?”
“No,” he responded. “I’m six-foot-four, but people tell me I look taller at night.”
As nurses continued to come in and out, hovering around and over me, I began to feel like I was being watched over by angels—or at least the closest thing to angels that one can find on earth. I then dropped into a half-sleep, only to be awakened by the sound of someone fiddling with my trash can. “Oh, I’m sorry if I woke you up,” she said.
“Actually, I’m glad to have you here. I’m feeling very anxious about my procedure tomorrow, and you are a nice distraction.”
Read related article: Bringing Integrative Medicine to the Ann Arbor Veterans Hospital
“That’s actually what I think my real job is,” she said. “I clean the rooms of people who are sleeping really fast so that I can spend more time with the people who need to talk to me. Are you missing your loved ones?”
“Yes, and tomorrow they’re going to cut me open for the third time in two weeks.”
“Well, I took this job just so I can talk with people like you. I find it meaningful to support people during Covid when they can’t have visitors. I think it’s especially terrible when people die alone here because their loved ones can’t see them. Those are the people I really wanted to help, but I found out they’re not able to talk with me because they’re so sick.”
“You mean you took a janitor job just so you can talk to people during Covid?”
“Yeah. But I’m not a janitor—I’m an environmental specialist. And I’m proud of what I do. Why don’t you go to sleep now? Tell me your name and I will pray for you. And you can be sure the doctors really know what they’re doing here. People come here from around the state, and even the Midwest. I know because I’ve talked with them. The doctors will do a good job for you.”
All through the night the angels came, and just knowing they were available at the push of a button helped me finally get some good sleep.
In the morning, the attending surgeon and her team came to go through their plan. I put my husband on the phone so he could hear her explain how my infection had happened. Apparently, bile contains a lot of bacteria, and a few drops of bile had fallen into a small amount of blood as doctors removed my gallbladder. The blood was the perfect place for the bacteria to grow, and now I had a large abscess that needed to be cleared away. The procedure went off as planned that afternoon, and I was released two days later.
During my follow-up visit, an attending surgeon told me that infections from gallbladder surgery at the U-M Hospital are so rare that they happen to only three to five patients a year. “When something like this happens, we doctors try to figure out why. Maybe we did something wrong. We are not gods, though some doctors might think that they are. We are mere mortals and sometimes we might make a mistake. We wonder if we could have prevented it. So, doctors cannot be perfect—as much as our patients might wish that we were. The only thing we are in total control over is kindness. If a doctor cannot be kind, he should go and work as a stockbroker. He has no place here.”
I almost told him about Dr. A. not giving me pain medicine, but I reminded myself that Dr. A. had apologized for that at least ten times. We had shaken hands on our agreement to be friends and I had made a promise to myself to forgive and forget. I had made a commitment to be kind.
By the day I was released, on May nineteenth, the state of Michigan was finally emerging from its third wave of Covid infections. Health officials attributed this to two factors: the warmer weather and mass vaccinations were lowering the daily case rate, so fewer people were exposed to the disease. For all their differences, many people in the state were pulling together to fight a common enemy. But there were still too many people who were left fighting for their lives inside hospitals around the state. And many, many healthcare workers would never forget what it was like to spend time with dying patients who could not see their family members. The pandemic left a scar that would never go away.
I was left with a wound that measured about three inches deep and two inches long after the infected tissue was cleared away. My scar is much smaller, but it, too, will never go away. And that’s okay. It helps me feel gratitude for all the people at the hospital who took such good care of me. And for the wisdom of my body, that knows so well how to heal.

































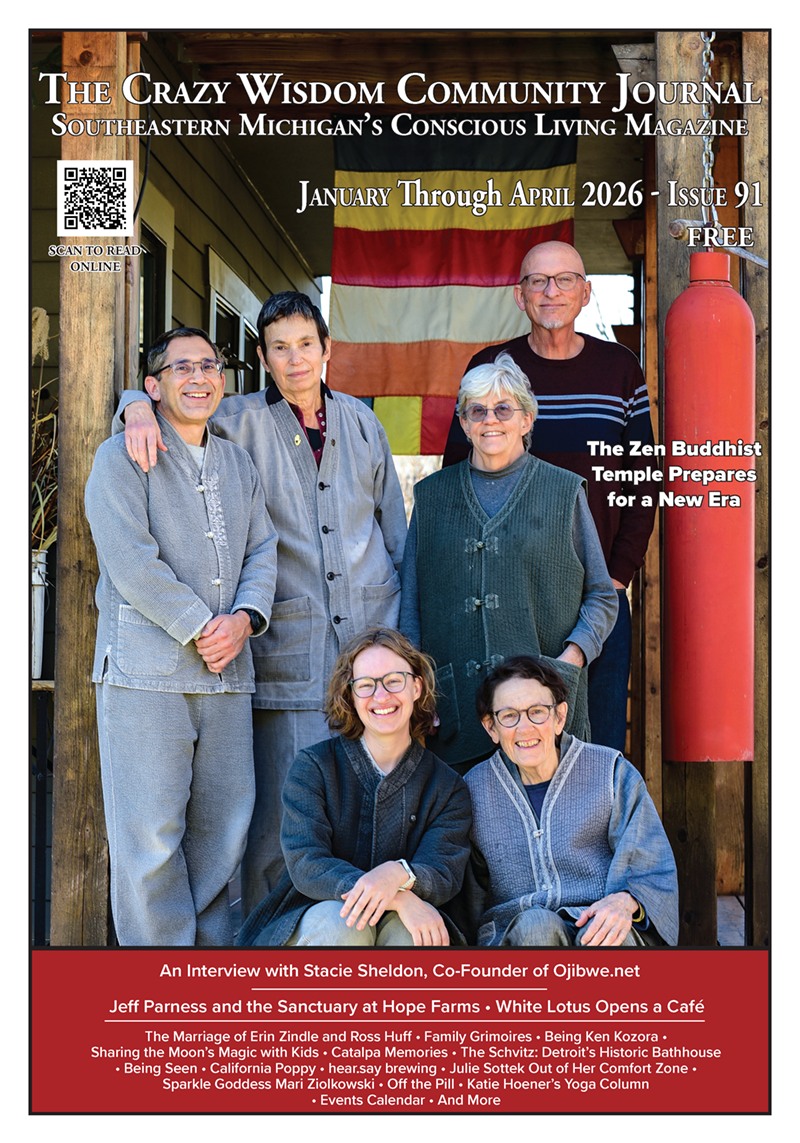



Recipes for Moon Milk and Harvest Lentil and Wild Rice soup. Winter Issue #91